Remote Monitoring - COPD
United4Health (U4H) was a European large scale deployment project that successfully implemented and assessed the impact of innovative healthcare services for the remote monitoring of patients with chronic conditions. The project included 10 countries one of which was Wales. At Hywel Dda University Health Board in West Wales they deployed telemonitoring which focused on managing and supporting patients with chronic obstructive pulmonary disease.
A comparison was made from the COPD Routine Care Service Model to the COPD Telehealth enabled model.

COPD Care Management - routine care
Patients with COPD who are admitted to hospital due to an exacerbation of their COPD are usually referred to the specialist home-visiting nursing service on discharge. The nurse, together with the patient’s GP, provide ongoing post-exacerbation care and support (Amber/Pink). The support is designed to enable the patient’s symptoms to stabilise and for them to self-manage (Green). Depending on the severity of patient’s COPD, ‘stable’ patients will be discharged from the specialist home-visiting nursing service and return to having their COPD care management from their GP and GP nurse. Routine care for all patients with COPD includes the offer of:
- Annual flu vaccinations
- Single dose pneumonia vaccinations
- Appropriate inhalers
- Spirometry, and MRC score review
- Pulmonary rehabilitation
- COPD Educational Programme for Patients,
- Non-invasive ventilation
- Home oxygen
- Palliation according to the severity of their disease.
Patients are able to be referred to medical and nursing COPD specialists in the hospital and/or community services if required (Pink).
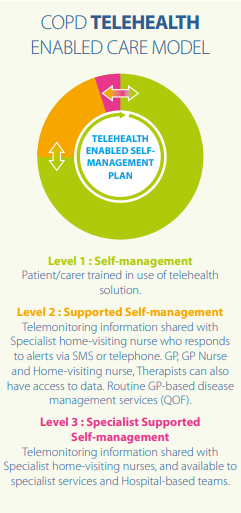
U4H Telehealth Enabled COPD Care Management
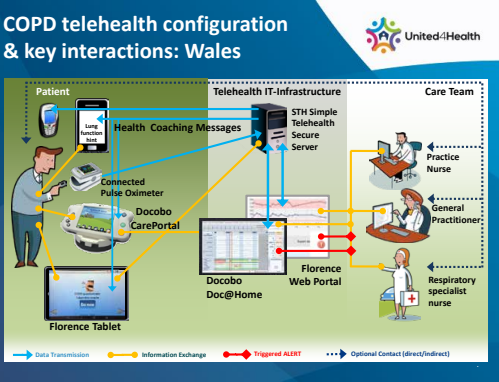
In comparison patients living with COPD enrolled into U4H project received either the Florence (NHS developed Simple Telehealth) - https://generatedhealth.com GPRS software system or the Docobo landline system (www.docobo.co.uk).
A patient or their carer performs the blood oximetry, temperature and symptom questions daily. The oximetry and temperature recordings are sent to the hub either via Bluetooth (Florence) or by wired connection (Docobo), and transferred to a computerised decision tree.
The symptom questions are responded to manually by the patient, and answers are entered, either by the patient or their carer via Flo/Docobo (Green).
For the first 7-10 days patients also received a daily telephone call from their specialist home-visiting nurse (Pink).
(A video conference was unable to be performed due to the lack of reliable broadband and 3G coverage).
The patient continued to take their vital signs and symptom questions for at least 30 days after commencing the telehealth service up to a maximum of 3 months (Amber).
Florence responded to the symptom question data according to an individualised set of parameters, and provided instant feedback to the patient via their computer tablet along with locally agreed advice messages every three days. The Docobo did not provide feedback direct to the patient. Alerts are sent to the patient’s key healthcare professional if readings and responses are outside the patient’s personalised parameters. The professional contacts the patient either by SMS or telephone (Pink).
After recovery from the initial exacerbation, patients are transferred on to the low intensity telemonitoring service and receive advice and motivational messages every three days (Green). Healthcare professionals can access the results uploaded to Flo and Docobo, via a secure internet connection, at any time.
Project Aims
- To offer patients living with COPD support of self-management through flexible telemonitoring that can respond with fluctuations in the patient’s health status.
- To avoid future emergency hospital admissions due to a COPD exacerbation following the support given.
- To procure any necessary technology, integrating it into existing health care services and redesigning pathways as necessary.
- Evaluate different aspects of deployment.
- To offer accessible, equitable and sustainable services to patients.
- To provide an insight into the challenges and opportunities that come from attempting to transform mainstream service delivery.
- Hywel Dda University Health Board
Conclusions
- With less than 1/3 of our target population in the final dataset, we feel that Telemonitoring following acute admission for COPD is currently not able to be implemented at scale under current conditions.
- Telemonitoring is safe and popular with users
- Telemonitoring confers some clinical benefit, probably in the longer term (data post 6 months appears more consistent-not shown)
- Telemonitoring shows mixed evidence of cost-effectiveness according to different settings
Link to document: Transforming the Experience for Patients Living with COPD: Services,Protocols and Results

